My Gluten-Free Nightmare: What Happens When a Celiac Eats Gluten
After 28 years on the planet, the last thing I’d expect is to receive a diagnosis of celiac disease. But roll back to July 2021; that’s precisely what happened.
In a way, it was somewhat of a relief. For years, I’d been struggling with what I thought were just some really annoying digestive issues. But it turns out those digestive issues were actually my body’s reaction to gluten.
So, what happens when a celiac eats gluten? In short, it’s not pretty. For me, eating gluten results in severe abdominal pain and cramping, bloating, gas, diarrhea, and fatigue. And unfortunately, that’s often just the tip of the iceberg.
Some people with celiac disease also experience headaches, brain fog, joint pain, anxiety, depression, and even skin rashes. The list goes on…
Let’s take a closer look at what happens when a celiac eats gluten and what you can do to avoid it.
What is Celiac Disease?
I’d forgive you if you haven’t heard of celiac disease before. After all, even in this day and age, awareness is still relatively low. But when you consider that it affects around 1 in 100 people [1], it won’t be surprising for awareness to increase significantly in the coming years.
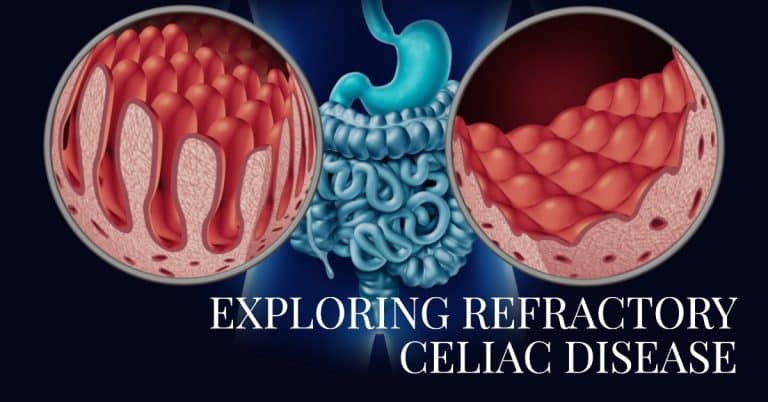
In case you weren’t aware, celiac disease is an autoimmune disorder that damages the small intestine when gluten is consumed. Gluten is a protein found in wheat, barley, and rye.
For people with celiac disease, consuming gluten triggers an immune response that attacks and damages the villi (tiny finger-like projections) in the small intestine. This damage prevents the absorption of nutrients from food and can lead to various health problems, including malnutrition, nervous system problems, and even cancer.
Celiac disease is often genetic, which means that if you have a first-degree relative (parent, child, sibling) with the condition, you’re more likely to develop it yourself. But it can also occur in people without a family history of the disease.
For me, it was the latter. Aged 28, I was diagnosed with celiac disease entirely out of the blue—no family history. I was just your average, run-of-the-mill person who one day found out that he could no longer eat gluten.
The Struggles of Being a Celiac
If there was ever a good time to receive a diagnosis of celiac disease, it would be now. Go back to say the turn of the century, the options for gluten-free living were pretty limited, and awareness was almost nonexistent.
If you so much as mentioned celiac disease to anyone while eating out, it wasn’t uncommon to be met with a blank stare. A gluten allergy or intolerance? Sure, perhaps they’d heard of that. But celiac disease? Probably not.
Thankfully, times have changed and awareness of celiac disease has grown exponentially. Restaurants are now much more likely to accommodate your needs, and the availability of gluten-free products has increased dramatically (albeit often at a premium price).
Of course, you’ll need to get used to planning ahead (if you haven’t already) and doing things like packing your own meals when traveling. But overall, living with celiac disease is doable in today’s world.
What Happens When a Celiac Eats Gluten?
Even the tiniest amount of gluten can cause a significant reaction in people with celiac disease. And no, I’m not being dramatic when I say “tiniest amount.” We’re talking about crumbs here.
You’ll know the drill if you received your diagnosis a while ago. For those of you who are newly diagnosed, you’ll need to be extra vigilant when it comes to avoiding gluten.
And it’s not just a case of scouring the ingredients list for anything that contains wheat or other gluten-containing ingredients. Cross-contamination is a real thing, and it’s something that you need to be aware of at all times.
For example, if you’re eating out, there’s a chance that your food could come into contact with gluten during preparation. The same goes for preparing food at home, too, especially if you share kitchen space with non-celiacs.
So what happens when a celiac eats gluten? For me, the effects are pretty much immediate. Within an hour or so of consuming gluten, I’ll start to feel nauseous, and my stomach will start to cramp up.
I have IBS (irritable bowel syndrome) on top of celiac disease, so the cramps can be pretty painful. It even hurts just to lie down!
After a few hours, diarrhea or constipation kicks in, and that’s usually when the ‘fun’ really starts. For the next few days, I’ll be pretty much confined to the bathroom as my digestive system tries to purge the gluten from my system.
As you can probably gather, it’s not a pleasant experience. But it is what it is, and unfortunately, when you’re ‘glutened’, there’s not much you can do other than ride it out.
How to Avoid Getting ‘Glutened’
Getting glutened is probably one of the worst things that can happen to a celiac. Not only is it incredibly unpleasant, but it can also set you back for weeks or even months in terms of your recovery.
So what can you do to avoid getting glutened? The best advice I can give is always to be vigilant and err on the side of caution. If you’re ever in doubt about whether something contains gluten, don’t eat it. It’s not worth the risk.
When eating out, tell your waiter or waitress about your celiac disease and ask them what steps they take to avoid cross-contamination. It won’t always be plain sailing, but it’s important to be as proactive as possible.
And finally, when preparing food at home, always take care to avoid cross-contamination. This means using separate chopping boards, knives, and pans for gluten-free and gluten-containing foods.
If you’re sharing kitchen space with non-celiacs, it’s also important to clean surfaces thoroughly after they’ve used them. A quick wipe-down with a damp cloth isn’t enough – you need to use hot soapy water to remove all traces of gluten.
Living with celiac disease can be tough, but it’s doable. With due care and attention, you can do your best to avoid getting glutened and enjoy a relatively normal life (with a few compromises thrown in for good measure!).
Disclaimer: This content is based on my personal experience as an individual diagnosed with celiac disease and IBS (Irritable Bowel Syndrome) who follows a strict gluten-free diet. This does not constitute medical advice. Please consult a medical professional, nutritionist, or qualified dietitian for personalized, professional advice.